Most persons who acquire hepatitis C virus (HCV) will develop chronic infection.[1] Following acute infection, HCV is very successful in establishing persistent infection by evading the immune system. Although the mechanism for the high rate of viral persistence is not completely understood, several viral and host factors play a significant role.[2,3] The actual rate of chronicity following initial infection with HCV is not well established in prospective studies, primarily because of the high percentage of persons who have asymptomatic or unrecognized early infection.[4] The chronicity rate has been estimated from cross-sectional population-based studies, such as the National Health and Nutrition Examination Survey (NHANES), as well as numerous retrospective studies.[5] Overall, it is estimated that 55 to 85% of persons who acquire HCV will develop chronic HCV infection.[6]
Role of Immune Response in Outcome of Early Infection
The rate of HCV production is high, 1010 to 1012 virions per day, and the lack of proofreading by the viral polymerase leads to enormous genetic diversity, which in turn creates a major challenge for the host immune response. This broad viral genetic diversity contributes to the high likelihood of developing chronic infection, whereas certain host factors play an important role in whether an individual will go on to spontaneously clear HCV.[7,8,9] Human and animal studies indicate that clearance of HCV is associated with strong and persistent HCV-specific cytotoxic T-lymphocyte and CD4 lymphocyte responses.[10,11] In addition, persons who clear HCV generally have limited viral diversity, which also points to enhanced immune-mediated response to acute infection.[12]
Host Factors Associated with Viral Clearance
The reason HCV infection persists in most patients but resolves spontaneously in others is not well understood. The following characteristics have been associated with a lower rate of chronicity.
- Younger Age: The rate of developing chronic HCV infection may be lower in younger persons, including those who acquire HCV during childhood.[13] In one study of 67 children infected with HCV through contaminated blood transfusions, only 55% developed chronic infection.[14] Similarly, in a prospective cohort that assessed viral clearance among 919 persons aged 17 years or older, there was a marginal association between age younger than 45 years and HCV viral clearance.[6]
- Female Sex: In a large retrospective analysis of more than 704 women who acquired HCV after receiving contaminated Rh immune globulin, 55% of the 704 women developed chronic HCV infection, a rate on the lower end of that typically reported.[15] In addition, several multicenter prospective studies of patients with acute HCV have reported women were more likely than men to experience spontaneous clearance of HCV.[8,16]
- Race: In the NHANES study, the rate of developing chronic HCV infection was determined by the prevalence of HCV RNA positivity among persons who had a positive HCV antibody test.[5] Overall, HCV viremia was present in 74% of persons with a positive HCV antibody test; however, the rate was 98% for African American men.[5] In a prospective cohort study involving 1,667 persons who inject drugs, African Americans were more likely to develop chronic infection than other races (91% versus 64%).[6] This racial difference in spontaneous clearance may be accounted for, at least in part, by differences in the IL28B gene (presence of CT and TT alleles) and other variations in alleles, which have been associated with a lower rate of spontaneous clearance and may be more prevalent among persons of African descent.[17,18,19]
- Symptomatic Acute HCV Infection: In a variety of studies, individuals who presented with clinical symptoms of acute HCV infection, particularly those who developed jaundice, were less likely to develop chronic infection.[3,4] It is believed that severe acute infection reflects a more vigorous immune response that results in higher clearance of HCV and thus a lower rate of chronicity.
- Absence of HIV Coinfection: In a prospective study of persons who inject drugs (PWID) who acquired HCV, those with HIV were more likely to develop chronic infection than those who did not have HIV.[20] In a subsequent study that enrolled persons with early HCV infection, HCV persisted in 95% of those with HCV and HIV coinfection and persistence was associated with relatively weak HCV-specific T cell responses.[21] Other studies have similarly shown relatively lower clearance of HCV in persons with HIV coinfection and one prospective study of viral clearance among 9,191 persons age 17 years and older found an association between lower CD4 count and decreased odds of HCV clearance.[22,23]
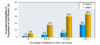
- IL28B CC Genotype: The single nucleotide polymorphism (SNP) rs12979860 is located upstream from the IL28B gene that encodes for interleukin 28 (also referred to as interferon lambda). Variations in the rs12979860 SNP have been associated with the probability of clearance of HCV.[17,24,25] Individuals with the CC allele of IL28B genotype are more likely to spontaneously clear HCV than those with CT or TT genotypes. In one report involving 1,008 individuals, those with CC genotype cleared the virus 53% of the time compared with a clearance rate of 23% for those with the TT genotype (Figure 1).[17]